What is a Middle Ear Infection?
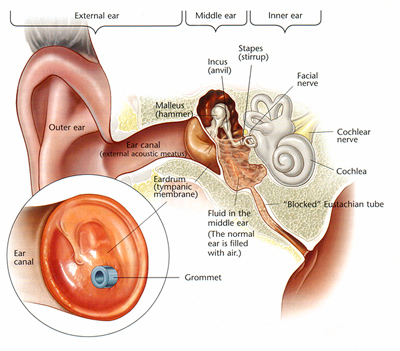
A Middle Ear Infection (also referred to as Otitis Media by healthcare professionals) refers to an infection, inflammation or fluid build up behind the eardrum.
Middle ear infections can either be acute or recurrent in nature. Recurrent Otitis Media is defined as 3 or more separate episodes of Acute Otitis Media within a 6 month period. Otitis media with effusion, also known as ‘glue ear’, describes fluid that remains in the middle ear after the infection has resolved. It is usually not painful, but does affect the child’s hearing ability.
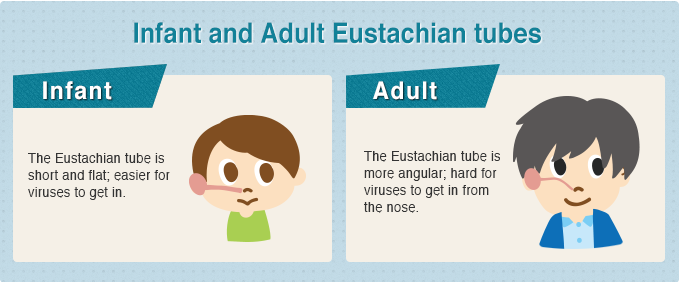
Middle Ear Infection is the most common childhood illness and is very common in children aged between 6 months and 4 years. This is due to the Eustachian tube being shorter and more horizontal than it is in older children and adults. The Eustachian tube is meant to help equalize the pressure in the middle ear and drain the fluid in the middle ear – when fluid cannot be drained and stays in the middle ear it is likely that it becomes infected.
Who is at risk for Middle Ear Infections?
- Children aged between 6 months and 4 years
75% of children will have at least one middle ear infection by the time they are three years old. Nearly half of these children will have three episodes by the time they are three years old
- Children who are bottle fed while lying flat
When children are being bottle fed, they should be propped up at a 20 degree angle, at least. This ensures that the milk does not flow back into the middle ear
- Children who have not been breast fed
- Children with prolonged dummy use
- Children exposed to smoke
- Family history of Middle Ear Infections
- Children with allergies
- Children who are more susceptible to colds and flu specifically those prone to sinus infections
Symptoms of a Middle Ear Infection
- Hearing difficulties
- Ear pain
- Tugging of one or both ears
- Difficulties sleeping
- Fever
- Loss of balance
- Irritability
- Discharge from the ear
What should I do? When should I get help?
Most cases of acute Middle Ear Infections should resolve by themselves. It is recommended that the child is treated for pain for the first 48 hours, however, if they symptoms worsen or do not improve then it is recommended that the child be seen by a doctor. The doctor will generally prescribe antibiotics. It is extremely important to complete the course of antibiotics. A child who has any discharge coming from their ear should see a doctor immediately.
If your child has had multiple cases of Middle Ear Infections it is recommended that you take your child to an Ear Nose and Throat Specialist (ENT), who will decide if grommets are necessary. Your child having grommets inserted is a relatively simple procedure that places small ventilation tubes within the ear drum. The grommets allow for drainage of fluid in the middle ear, let air into the middle ear as well as equalise the pressure between the middle ear and the ear canal.
All children who have suffered with Middle Ear Infections should be taken for a full diagnostic Audiological evaluation with an Audiologist once the middle ear infection has been resolved.
What to expect from an Audiologists visit
The audiologist will conduct a full comprehensive Audiological evaluation which will include an in-depth evaluation of your child’s outer ear, middle ear and inner ear. The Audiologist will complete the following examinations:
Otoscopy
An Otoscopic examination is used to visualize the ear drum. During this assessment, the audiologist will be able to see if there is still presence of a Middle Ear Infection or if the ear drum has burst during the ear infection.
Tympanometry
Tympanometry is an examination used to test the middle ear volume and pressure. During this assessment the Audiologist will be able to see if there is a middle ear infection present, if the ear drum is intact and if the pressure in the middle ear is normal.
Audiometry
The Audiologist will then conduct a pure tone audiometric examination. During this test, the audiologist will be able to determine your child’s current hearing ability and if any damage has occurred to your child’s hearing by the ear infection.
Middle Ear Infection complications
The following complications may arise from Middle Ear Infections:
- Burst ear drum
In severe cases of Middle Ear Infections the fluid build-up puts too much pressure on the eardrum and subsequently causes the ear drum to burst (hole in the ear drum). This can either heal by itself over time or the ENT may deem surgery necessary to repair the hole.
- Delayed speech and language
During an ear infection the child’s hearing is reduced by 24-45 dB. Their hearing is similar to how you hear while under water or with foam earplugs in your ears. This is a crucial time for speech and language development. If a child is not getting adequate speech and language input due to their decreased hearing, their speech and language development may become delayed. In these cases, it is important to seek professional help from a speech-language pathologist as soon as possible.
- Permanent hearing loss
In some cases when there have been too many occurrences of Middle Ear Infections or the damage from the infections is too extensive, it may cause permanent hearing loss. In these cases a hearing aid may be beneficial. It is important to seek professional help from an Audiologist as soon as possible
Prevention of Middle Ear Infections
- Never bottle feed your baby, while they are lying flat
- Avoid exposing your child to second hand smoke
- Keep up to date with your child’s recommended immunisations
Although some preventative measures can be taken, it is important to note that if a child is susceptible to Middle Ear Infections, there is very little that can be done to completely avoid them. If you are worried about your child’s hearing or speech development, it is important to consult a medical professional.
- Dangerous Decibels, Noise induced hearing loss in children - June 14, 2019
- Listening to Learn - April 17, 2019
- Listen Up! What’s the big deal with childhood hearing loss? - February 8, 2019



1 thought on “Exploring Middle Ear Infections”
Your post is a breath of fresh air. The content is unique, and your perspective is refreshing.