Sleep is so essential for our children’s overall development and health, but we cannot address sleep habits if there are medical reasons for a child’s restless nights. There are a few ear, nose and throat (ENT) related conditions that can contribute to poor sleeping – let’s look at the two most common causes amongst infants and toddlers:
Adenoid hypertrophy or enlargement
Any form of a blocked nose causes difficult, uncomfortable and noisy breathing while sleeping. The most common cause for a chronically blocked nose that an ENT specialist diagnoses are enlarged tonsils and adenoids.
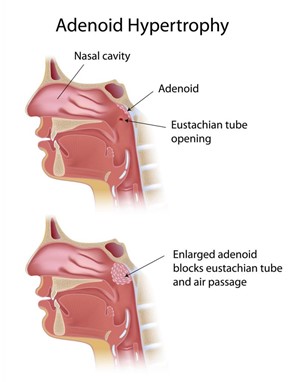
Adenoids are lymphoid glands that form part of your immune system. They are located behind the nasal cavity where they trap viruses and bacteria or allergens that try to enter and infect the upper respiratory tract. When they are constantly exposed to viruses or bacteria (for example at creche or school) or even to allergies, they enlarge and block the passage where air needs to pass from the nose to the airway. Adenoids are often enlarged in children, but shrink as we grow older and our immunity improves. Adenoid hypertrophy causes snoring, a blocked and runny nose, nasal voice, mouth breathing and postnasal drip with night-time wet coughs.
Severe cases can even lead to obstructive sleep apnoea where your child stops breathing for a few seconds at a time. Your child will snore loudly and wake sporadically during the night due to these pauses in breathing and will not be able to enter the deeper part of sleep. In the long run this is detrimental to their sleep and overall health as essentially, they are not getting enough oxygen to their bodies and their hearts and lungs must work extra hard. It can lead to failure to thrive and poor growth, behavioral problems, poor school performance due to lack of concentration, enuresis (bed wetting) and even heart failure.
Middle ear infection or effusion
The middle ear has a natural drainage pathway to the back of the nose called the eustachian tube. Any fluid build-up in the ear from inflammation or an ear infection is supposed to drain naturally via the eustachian tube. When the adenoids are enlarged and block the eustachian tube’s opening, this cannot occur and fluid builds up and becomes stagnant in the middle ear. This leads to recurrent infections or chronic fluid build-up called an effusion. You know the feeling you get when your ears need to pop when landing in an aeroplane? That is the pain a child has almost constantly when there is pressure build up in their middle ear, especially when lying down and there is increased blood flow to the head. That is enough to keep anyone awake at night.
Not only is it painful for children, but it can cause difficulty in hearing and eventually delay their speech development because of the muffled sounds. In severe cases it can even affect their balance. Some mothers notice how their infants walk differently when their ears are acting up.
These conditions are very common in infants from around 6-8months of age into toddlerhood and if the above symptoms are present, it’s best you visit an ENT specialist. There are certain medications that can be prescribed if caught early to try and reverse the inflammatory process and essentially shrink the adenoids, but often it requires surgery. The surgery is a low-risk, quick procedure where the adenoids are removed through the mouth (often combined with a tonsillectomy) and grommets can be inserted into the eardrums to drain the fluid.
Once these medical conditions have been resolved there will be a marked improvement in their sleep and a child that already had well-stablished sleep habits, will often return to sleeping well once they are feeling better.
What can you expect from their sleep once they have been treated?
Waking early:
Suffering from any of these conditions affect both the quality and quantity of your child’s sleep. Some children become so accustomed to poor quality sleep that once they finally get helped, they find themselves waking up at the crack of dawn refreshed and ready for the day. They’ve never slept so soundly before, and it can take your child a while to adjust to sleeping more appropriate hours.
White noise:
Once ears are cleared of fluid, some children become hyper-sensitive to the white noise in their room. You can temporarily reduce the volume and remember to never exceed 50 dB once you turn the volume back to normal.
Discomfort:
This will need to be addressed and you should offer your child comfort and reassurance. Once they are feeling better go back to your plan and ensure that they don’t become reliant again on any unsustainable sleep associations. Short term-use is often not the problem, it is allowing the bad habits to creep back in permanently that becomes an issue.
Once your child is feeling better and has recovered, go back to their normal routine. Often sleep concerns after a procedure are easily resolvable and your sleep-trained child will undoubtedly surprise you with how well they bounce back.
If your child slept poorly prior to the procedure, look at contacting a sleep consultant for some assistance. Quality sleep is vital to your child’s health and well-being and they certainly deserve a good night’s rest after what they’ve been through.
By Dr Nina du Toit – ENT and Tammy Buitendach – Good Night Consultant

For more help on sleep related matters for your baby and/or toddler, contact [email protected], www.goodnightbaby.co.za or like the Facebook page http://www.facebook.com/GoodNightbabyrsa
- “Sleep When Your Baby Sleeps” – Planning for Newborn Sleep Bliss - March 18, 2024
- WHERE SHOULD YOUR BABY SLEEP? - March 11, 2024
- Don’t get “nap trapped” - March 5, 2024





